Intestinal Obstruction
One difficult and potentially dangerous condition that stands out in the complex field of gastrointestinal health is an intestinal obstruction. By discussing the definition, causes, symptoms, diagnosis, and significance of prompt intervention for successful management, this blog seeks to clarify the intricacies surrounding intestinal obstruction.
 |
| Intestinal obstruction |
A condition known as bowel obstruction occurs when the bowels become narrowed and unable to function normally. The constriction could be brought on by a malignant tumour or colon inflammation. Food particles cannot pass through the bowel (tube) if it becomes blocked, which could result in symptoms.
Intestinal Obstruction Causes:
- After abdominal surgery, scar tissue may form, which may cause the intestines to adhere to one another and obstruct flow.
- An obstruction could result from a section of the intestine poking through a weak spot in the abdominal wall.
- The normal flow may be impeded by benign or malignant growths in the surrounding tissues or within the intestine.
- It is possible for the colon to twist on itself, obstructing the blood flow and causing a blockage.
- Conditions such as diverticulitis or Crohn's disease can cause inflammation, which can then result in blockage.
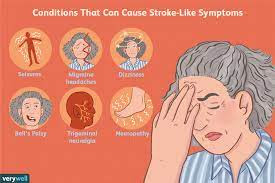
Symptoms of intestinal obstruction
It is essential to recognise the symptoms of intestinal blockage in order to get medical help as soon as possible. Typical signs and symptoms consist of:
- Lower abdominal pain, either intermittent or constant, can cause cramping.
- Vomiting may result from an inability to pass gas or stool.
- Abdominal distension and swelling brought on by trapped fluid and gas.
- inability to pass stool or lack of bowel movements.
- a discernible decrease in gas passage.
Diagnosis & Treatment
Intestinal blockage diagnosis is made by combining medical history, physical examination, and diagnostic imaging tests (endoscopy, CT scan, or X-ray). Prompt medical intervention is imperative upon identification in order to avert complications like ischemia and bowel perforation.
To remove the fluids and gas from the patient's intestine, it is imperative to keep them off of food and to use a nasogastric tube.
The patient will receive intravenous fluids to treat their dehydration and maintain normal electrolyte levels.
Patients may occasionally receive medication to treat underlying infections that are the cause of their problems, and if other treatments are unsuccessful, surgery may be performed.
To remove a bowel obstruction, surgery may be necessary. This could include stoma formation, adhesiolysis (adhesion release), intestinal resection, or a bypass surgery. In order to suture (join) the two ends of the bowel together, surgeons may remove the damaged section. They will make an abdominal incision to remove the bowel's end, and a stoma bag will collect your stool if the two ends cannot be joined.
Metallic tubes, also known as stents, called self-expanding metal stents (SEMS) are used to hold the colon open when a tumour obstructs it so that stools can pass through.
Recovery Phase
Intestinal obstruction recovery frequently entails a mix of lifestyle and medication changes. Recurrence must be avoided by post-treatment, dietary changes, and routine check-ups with medical professionals.
Take away point
Being aware of the symptoms and risk factors can encourage people to seek care as soon as possible, increasing the likelihood that their treatment will be successful and reducing the likelihood of complications such as intestinal perforation or aspiration of bowel contents into stomach.For a comprehensive assessment and individualised care, speak with a medical professional if you believe you may be experiencing symptoms of intestinal obstruction.